What is Angioplasty?
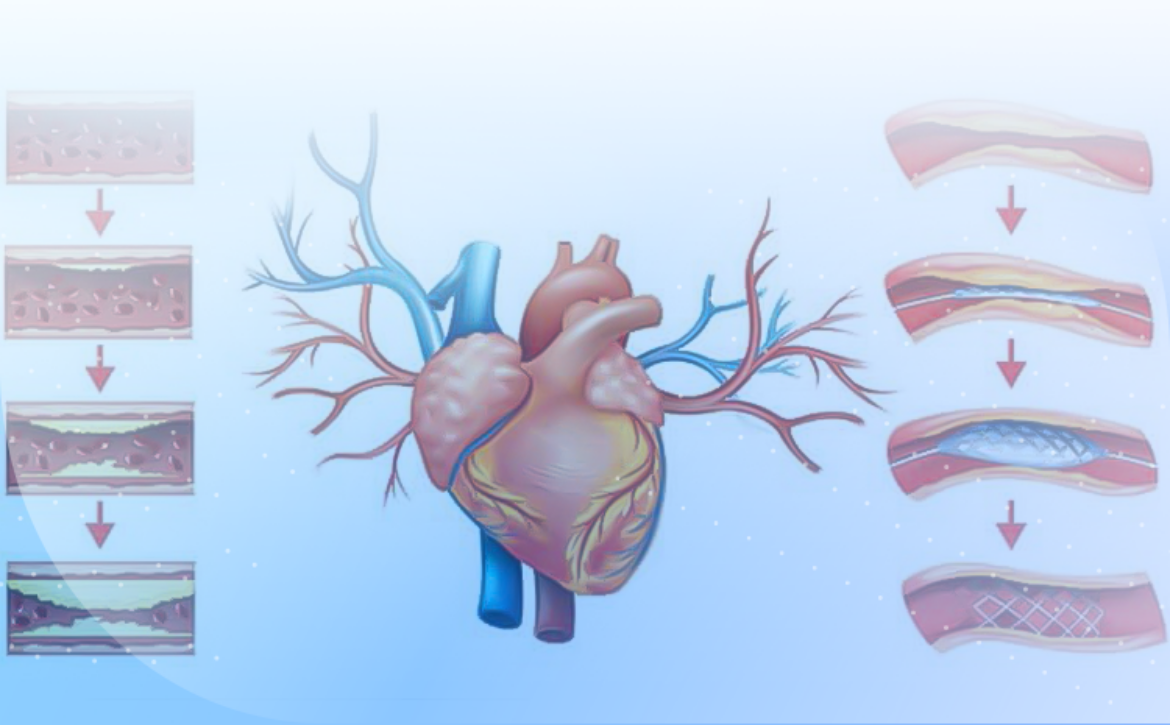
Angioplasty is a medical procedure used to open narrowed or blocked blood vessels, particularly in the heart. This method is primarily employed to treat cardiovascular diseases, such as coronary artery disease (CAD).
- History
Angioplasty was first introduced in 1977 by Dr. André Gruntzig, a cardiologist. Since then, this procedure has been widely used in the treatment of vascular problems, with significant advancements in technology and techniques.
- Procedure of Angioplasty
Angioplasty is typically performed as follows:
-
Preparation: The patient is usually given local anesthesia and may also receive sedation.
-
Accessing the Vessels: A catheter (a thin, flexible tube) is inserted through a blood vessel in the arm or leg and guided towards the coronary arteries.
-
Imaging: Using X-rays and a contrast agent, the doctor can visualize the condition of the blood vessels.
-
Opening the Vessels: A small balloon at the end of the catheter reaches the site of narrowing or blockage and inflates to open the vessels. In many cases, a stent (a mesh tube) is also placed at the site of narrowing to prevent re-narrowing.
- Advantages and Disadvantages
Advantages:
- Improved blood flow to the heart
- Reduced symptoms of heart disease, such as chest pain
- Enhanced quality of life
Disadvantages:
- Side effects such as bleeding, infection, or allergic reactions to the contrast agent
- Possibility of re-narrowing of the blood vessels
- Post-Angioplasty Care
Patients typically require special care after undergoing angioplasty. This includes taking blood-thinning medications, making lifestyle changes, and having regular follow-ups with their doctor.
- Conclusion
Angioplasty is an effective procedure for treating vascular issues that can help improve the quality of life for patients. However, like any medical procedure, it requires careful evaluation and consultation with a specialist physician.